In a candidate for coolest experiment of the year, scientists at Stanford University surgically created conjoined-twin mice of different age pairs to assess the impact of young versus old blood on the brain.
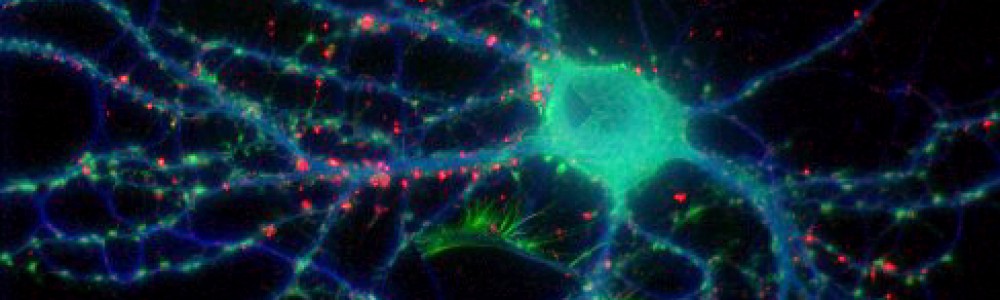
Published this month in Nature, researchers investigated the effect of proteins in the blood to encourage or inhibit neurogenesis (new cell growth in the brain), concentrating on the dentate gyrus of the hippocampus, a key area in memory consolidation and a region known to be susceptible to environmental and age-related changes in cellular growth and death. The hippocampus is strategically located in an area rich with blood vessels, making it an ideal region to look for the effects of aging blood on the brain.
First, looking at older mice, scientists identified a decrease in neurogenesis and synaptic plasticity, as well as behavioral learning and memory, confirming deficits commonly seen in aging populations.
Next, using a procedure called parabiosis, pairs of young and old mice were surgically attached to one another, enabling the sharing of blood, plasma, and proteins between the two through their newly conjoined cardiovascular systems. In the heterochronic condition (unions of young to old mice), significant differences in the levels of new neurons and progenitor cells (similar to stem cells) were seen in each of the pair members. Older heterochronic mice had significant increases in these levels as compared to their isochronic paired counterparts (unions of old to old mice), whereas the unlucky younger mice of the heterochronic pairs saw significant reductions in the number of these new cells compared with the young isochronic mice. Additionally, extracellular recordings were taken from the heterochronic pairs, and a decrease in long-term potentiation–an indicator of the cellular plasticity essential in learning and memory–was decreased in the young heterochronic mice but increased in the older ones, further indicating the deleterious effects of old blood on the brain.
To confirm that the aging effects seen were due to proteins in the blood of these animals, a different set of young mice were injected with the plasma from either young or old animals. Again, young mice injected with the plasma from older mice saw decreases in the number of new cells in the dentate gyrus, indicating impairment in neurogenesis, whereas no differences were seen in the animals who were given younger blood. Behaviorally, these young blood recipients showed no changes in their learning and memory abilities, however, the mice who received the plasma from older mice now exhibited impairments in their fear conditioning and spatial learning behaviors similar to those seen in aging populations.
Finally, using a method known as a proteomics, researchers attempted to identify the individual proteins that might be causing these aging effects. They measured the levels of 66 individual proteins in the plasma taken from young and old mice and then compared them to the heterochronic pairs. In normal aging mice, 17 of these proteins were identified as being negatively correlated with neurogenesis, an increase in the proteins signifying a decrease in new cell generation. Increases in these specific protein levels across aging seem to inhibit neurogenesis, and 16 of these proteins were also found to be elevated in the young heterochronic paired mice. The team then narrowed down the field to one particular protein, CCL11, which is also known to have an age-related increase in humans. Scientists performed one last experiment to confirm the role of CCL11 in aging, injecting the protein into mice. This resulted in the anticipated increase in CCL11 levels in plasma, as well as a corresponding decrease in neurogenesis and new cells in the hippocampus.
The depth of this study, including the variety of different methods the researchers used, is one of the most impressive things about it, independent of the exciting discoveries they have made. Additionally, the idea of pinpointing a specific protein to stave off aging is one that keeps popping up in science, and the fact that CCL11 has been shown to have aging effects in humans as well as mice suggests that this might be a promising one to target. Or, on the flip side, we might see an unfortunate increase in geriatric vampire literature as a result of these findings. You never know.