I watched a good ‘psychological thriller’ the other night – Side Effects by Steven Soderbergh – that centers on a woman’s debilitating depression and critiques the pharmaceutical industry’s untoward influence over clinicians (it turns into a plot-twisty crime thriller, but that’s beside the point). The film got me thinking about our reliance on psychotropic medications to treat psychological distress, and how helpless we are when these pills don’t work.
I’ve written before on the over-medicalization of psychiatric disorders and the pharmaceutical industry’s role in this controversy, but this time the topic got me thinking about possible alternative treatments for depression, other than cognitive-behavioral therapy or mood-altering medications.
One innovative method for treating depression that has received attention is sleep deprivation. Acute sleep deprivation has been touted as having a 60% success rate in immediate relief from depression; however, this effect is temporary, only lasting until you finally do nod off.
At first this might seem surprising, after all, think about how cranky and irritable you feel after a poor night of sleep. But complete deprivation (i.e. missing an entire night’s sleep, or more than 12 hours) can actually have the opposite effect. Remember that loopy, giggly, hysterical feeling you used to get staying up all night at a sleepover, or at 5am in the library while studying for exams? It is believed that this phenomenon is at least partially caused by an alteration in activation and connectivity in our frontal cortex, potentially offsetting the harmful effects chronic depression can have on this area.
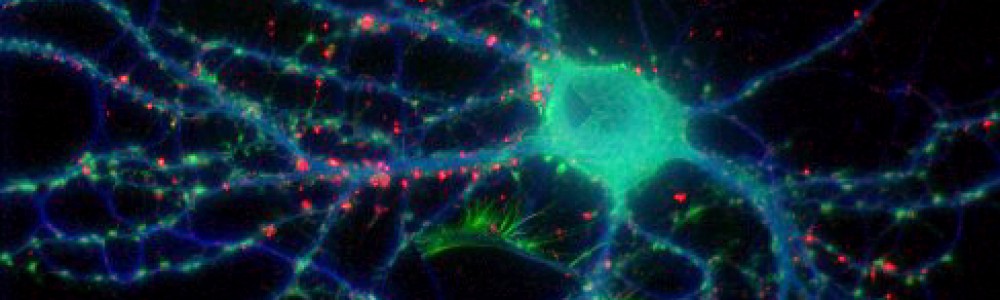
It is still relatively unknown how or why exactly this works though. A recent study from Tuft’s University attempted to answer this question by testing sleep deprivation and its efficacy as an anti-depressant in depressed mice. First, researchers confirmed that depressed animals who were sleep-deprived for 12 hours displayed significantly less depressive symptoms than control depressed mice. Then, for the first time, they were able to link this effect to the activation of a certain type of brain cell, astrocytes, that release a particular protein, adenosine.
Adenosine is important in sleep regulation, and its absence has also been implicated in a greater risk for depression. Adenosine release is increased the longer you’re awake (to a point), making you feel less aroused and more tired, and acting as part of your normal sleep-wake cycle. A beneficial side effect of its release now also appears to be an alleviation of depressive symptoms. However, after 72 hours of sleep deprivation there was no change in adenosine levels, as the astrocyte cells had largely shut down by this point. Thus, there was no effect of more extreme sleep deprivation on feelings of depression. Also, as soon as you do catch up on some zzz’s your adenosine levels return to normal and the anti-depressant effects disappear.
Adenosine’s effect on depression potentially works by altering the electrical signals in your brain, causing an immediate change in mood and behavior. Other fast-acting, unconventional treatments for depression, like deep brain stimulation and electro-shock therapy, are thought to work in a similar manner, impacting the brain’s electrical currents. These treatments also last much longer, suggesting that there may be a way to channel adenosine’s electrical effect into a longer-term solution.
I should be clear that I am in no way against using psychotropic medication to treat psychiatric disorders; in fact, in many instances these pills are absolutely essential. But in cases where these medications don’t work, or where their Side Effects are too severe (seriously, go see the movie!), it is important to have well-researched alternatives to the standard course of treatment. Also, it’s always nice to know how to get a good natural high every now and then, if you can stay up that long.
(Originally posted on Mind Read)